
|
|||
|---|---|---|---|
|
|
Hallux valgus: physical therapy treatment Hallux valgus: tratamiento fisioterapéutico |
|
|
|
Student of Physical Therapy La Laguna University, Tenerife (Spain) |
Orlando Pérez San Juan |
|
|
|
Abstract Introduction: The purpose of this article was to show a basic comprehension of the hallux valgus pathology through a brief review. Hallux valgus is an irreversible foot deformity. The condition, which in lay terminology is called “bunion,” is characterized by a lateral deviation (abduction) of the hallux with a corresponding medial deviation (adduction) of the first metatarsal. Deformity disrupts the normal straight alignment of the first metatarsophalangeal (MTP) joint. Factors like anatomy, pathomechanics and etiology were reviewed. Material and Methods: four articles were selected by an electronic search using the terms “hallux valgus conservative” and “hallux valgus physical therapy”. Results: it is presented a rehabilitation program based in the evidence and the multidisciplinar aspect of the treatment. Discussion: the treatment needs one global method because of the multiples factors implicated (muscle imbalances, cosmetics reasons or structural, among others). Keywords: Hallux valgus conservative. Hallux valgus physical therapy.
Resumen Introducción: El propósito de este artículo fue mostrar una comprensión básica de la patología Hallux Valgus a través de una breve revisión. Hallux Valgus es una deformidad irreversible del pie. La afección que es llamada “juanete”, se caracteriza por una desviación lateral (abducción) del hallux valgus con una correspondiente desviación medial (aducción) del primer metatarso. La deformidad altera el normal alineamiento de la articulación metatarsofalángica (MTP). Factores como anatomía, patomecánica y etiología fueron revisados. Material y Métodos: cuatro artículos fueron seleccionados mediante búsqueda electrónica empleando los términos “hallux valgus conservative” and “hallux valgus physical therapy”. Resultados: es presentado un programa de rehabilitación basado en la evidencia y aspecto multidisciplinar del tratamiento. Discusión: el tratamiento necesita un método global debido a los múltiples factores implicados (desequilibrios musculares, razones cosméticas o estructurales, entre otros). Palabras clave: Hallux valgus. Fisioterapia. Tratamiento conservador.
Recepción: 14/10/2015 - Aceptación: 17/11/2015
|
|||
|
|
EFDeportes.com, Revista Digital. Buenos Aires, Año 20, Nº 210, Noviembre de 2015. http://www.efdeportes.com/ |
|
|
1 / 1
Introduction
Hallux valgus (Fig. 1) is an irreversible foot deformity. The condition, which in lay terminology is called “bunion,” is characterized by a lateral deviation (abduction) of the hallux with a corresponding medial deviation (adduction) of the first metatarsal. Deformity disrupts the normal straight alignment of the first metatarsophalangeal (MTP) joint.
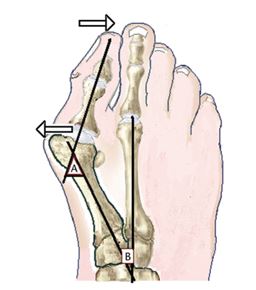
Figure 1. Hallux valgus disrupts normal alignment of the metatarsophalangeal joint. Arrows indicate the direction of joint member deformity displacements. The hallux abducts
while the first metatarsocuneiform segments adduct. The severity of the hallux-metatarsal deformity is measured by (A) hallux valgus angle and (B) intermetatarsal 1-2 angle
“Bunion” is a Latin word meaning enlargement, which refers to the chronic swollen appearance of the medial projected eminence that develops as the hallux deviates laterally into deformity. Pain, when experienced, is usually localized to the swelling (bunion) or in the first MTP joint itself. Shoes may aggravate the condition. The progression of hallux valgus, although not well understood, is predictable. The tensile strength of the medial collateral ligament of the first MTP joint weakens and the hallux abducts laterally into valgus. Coincident with abduction of the hallux, the metatarsal shifts medially into adduction, potentially subluxating the sesamometatarsal articulation.
The prevalence of hallux valgus is highest in the female populations living in Western societies that wear fashionable shoes. Shoes worn by women typically have a high-heel and narrow toe box. Heeled shoes increase pressure borne by the forefoot and, when worn over prolonged time periods, may lead to adaptive shortening of the ankle plantar-flexor muscles. Decreased ankle dorsiflexion, by itself, is considered a factor in hallux valgus.
Greater than 60% of patients having hallux valgus show a family history of the deformity. Congenital neurological pathology, such as ankle equinus associated with cerebral palsy, and chronic inflammatory conditions have been found to be related to hallux valgus. Damage of the first MTP joint occurs in nearly 25% of patients having rheumatoid arthritis (RA). Arthritis weakens the articular tissues, leaving the weight bearing joints at risk of dislocation; collapse of the arch is common.
Shape of the first metatarsal head also has been explored as a potential predisposition of hallux valgus. A flattened head is considered to be resistive to deforming forces, whereas a round head is thought more prone to allow the hallux to drift into deformity.
Sufficient evidence exists to show that first metatarsal mobility is increased in individuals having hallux valgus and that a large intermetatarsal 1-2 angle is an indicator of first metatarsal hypermobility.
Generalized joint laxity is a significant predictor of first metatarsal hypermobility. Patients having hallux valgus demonstrate a high incidence of multijoint laxity.
Material & methods
-
Literature search: an electronic search.
-
Databases: PubMed.
-
Key Words: hallux valgus conservative, hallux valgus physical therapy.
-
Date: 27 September 2015.
-
Inclusion criteria: filters
-
Species: Human.
-
Publication dates: custom date range: 2009/ 01/ 01 to 2015/ 12/ 31.
-
Languages: English.
-
Text availability: Full text
Table 1. Retained for literature review.

Results
To reduce discomfort, individuals having hallux valgus are advised to avoid wearing high-heeled, pointed-toed shoes. Shoes made from soft leather that is flat in style work best and if necessary, the toe box can be stretched to accommodate for bunion enlargement.
Regardless of the treatment applied, current available evidence indicates that deformity will progress until fixed by surgery (Glasoe et al, 2010).

Figure 2. SERI Technique. A 44-year-old woman with moderate hallux valgus.
(A) Preoperative radiographic aspect of the deformity.
(B) Postoperative radiographic view showing the osteotomy and the correction maintained by the Kirschner wire.
(C) Radiographic aspect at 7-year follow-up showing the correction of the deformity with
complete healing of the osteotomy and remodelling of the metatarsal bone (Giannini et al, 2013)
The use of toe spacers and splinting to stretch tissue tightness. Foot orthoses also may be incorporated into treatment (Giannini et al, 2013).
Therapy for hallux valgus aims to correct the forces acting on the first MTP joint. Suggestions for care include foot exercise to rebalance muscle strength (force-generating capacity) (Glasoe et al, 2010).
Rehabilitation Program (Schuh et al, 2009)
Cryo-cuff (Aircast, DonJoy Orthopaedics, Austria) was applied for 8 hours starting immediately after surgery and on the first postoperative day. This treatment was conducted as an inpatient treatment. Postoperatively, patients were placed in the Rathgeber (OFA Bamberg GmbH, Bamberg, Germany) postoperative shoe for 4 weeks. This shoe allows weight bearing of the operated limb while reducing stress of the forefoot region. Patients also received a special sock (Gilofamed, OFA Austria, Salzburg, Austria) that reduces swelling and the need for dressing changes. Physical therapy treatment same treatment started at 4 weeks after surgery, and there was one session per week.
Session 1
In the first session, elevation of the leg, lymphatic drainage, activation of the muscle pump, and cryotherapy (cool packs) were used to reduce the swelling.
Lymphatic Drainage: Each patient was placed in the supine position. Lymphatic drainage was performed starting from the anterior cervical region at the fossa supraclavicularis using the poncage technique (careful friction) to stimulate the supraclavicular lymph nodes in order to increase autonomic rhythmic contractions of these nodes. Additionally, the patient was instructed to perform deep inspiration with the therapist’s hands on the lower rib cage. The aim of this intervention was to stimulate the diaphragm to increase lymphatic flow toward the cisterna chyli and thoracic duct. The next step was to use the technique described previously for the inguinal lymphatic nodes for continuing with the adductor region, stimulating the popliteal region (popliteal lymphatic nodes) and the calf. After this the therapist started working around the malleolar region and forefoot and finished with a couple of effleurages from the toes to the inguinal region.
Activation of the Muscle Pump: plantar flexion and dorsiflexion of the ankle as well flexion and extension of the hip and knee.
Scar Tissue Massage.
Cryotherapy: was performed with ice or cool packs at the first metatarsophalangeal (MTP) joint region as well as the forefoot.
Mobilization: was performed at all MTP joints. These manipulations focused on the improvement of plantar flexion for MTP joints 2–5 and on the improvement of dorsiflexion for the first MTP joint. They included caudal sliding of the proximal phalanx to improve plantar flexion and dorsal sliding of the proximal phalanx to improve dorsiflexion (Fig. 3).

Figure 3. Manual therapeutic intervention at the first metarsophalangeal joint
Manual Therapeutic Interventions: oscillating traction was performed to activate the mechanoreceptors that inhibit the afferent pain sensors. The main region of this treatment option was the MTP joints. The proximal hand was placed close to the MTP joint line in order to stabilize the metatarsus, while the distal hand was placed on the proximal phalanx.
Gait Training: in this session, the main goal of gait training was to reach optimal load distribution for the whole foot during the entire stance phase, with special focus on weight bearing of the first MTP joint and hallux.
Session 2
Mobilization: mobilization of the MTP joints was performed as described for the first session. Additionally, pronation of the forefoot while stabilizing the calcaneus was performed. The physical therapist also performed isolated caudal glides of the navicular toward the talus, the cuneiform toward the navicular, and the first metatarsal toward the cuneiform. For this treatment, the patient was placed in a supine position. The physical therapist’s distal hand stabilized the plantar aspects of the manipulated regions, while the proximal hand was applying longitudinal force focusing on the specific joint (imitating the translating movements in the metatarsus). These mobilization exercises also could be performed in a sitting position.
Soft-Tissue Techniques: they were performed on the flexor hallucis longus, adductor hallucis (oblique and transverse heads), abductor hallucis, and tibialis anterior muscles to increase blood flow and decrease tension. Also, soft-tissue techniques on the peroneal fascial loge (especially in the tendinous region of the muscle) were performed in combination with active pronation in a supine or sitting position.
Motor Learning / Strengthening Exercises: muscle imbalance between the abductor hallucis (AbdH) and adductor hallucis (AddH) has been demonstrated in hallux valgus (HV). The toes-spread-out (TSO) exercise can be recommended for preventing or correcting HV deformity at an early stage (Kim et al, 2013) (Fig. 4).

Figure 4. Sequence of TSO exercise
The aim of these exercises was to strengthen the lumbrical, interosseous, adductor hallucis, peroneal longus and brevis, and flexor hallucis longus and brevis muscles. The patients had to learn to selectively activate one of these muscles and avoid using the flexor digitorum longus muscle in order to decrease pressure on the MTP joints (eg, patients had to plantar flex the MTP joint without bending the distal and proximal interphalangeal joints). Then the exercise was combined with active pronation. To increase strength, this exercise can be performed with an elastic band (Thera-Band). At the beginning, the patients did the exercises in a positive dynamic manner. When the patients became stronger, the exercises were performed as eccentric training.
Pronation is essential for ground contact of the first ray, the most heavily loaded structure of the foot during gait. If the peroneus longus muscle is too weak, people compensate by pushing the knee into a valgus position to achieve midfoot pronation. In addition, fascial release techniques for the peroneal muscles as well as to decrease of the tone (velocity-dependent resistance to stretch) of the tibialis anterior muscle were performed to improve the interaction of those antagonists.
Concentric strengthening exercises of the great toe flexors and extensors were performed as well.
The participants also were instructed to do a marble pick-up exercise.
Gait training
The previous learned understanding of functional muscle control of the transverse arch of the forefoot then was trained in mid-stance as well as the terminal stance position while standing. The focus was the active participation of push-off (barefoot).
Session 3
Sensomotoric Training: Intermuscular and intramuscular coordination was the goal of this treatment modality. Exercises were performed mainly in a standing (mid-stance) position, with increasing load on the weight-bearing foot and going into the one-foot position, controlling the foot, the knee, and the hip in a neutral long-standing leg axis (meaning the weight is distributed on the lateral aspect of the heel and MTP 1 and 5 with the knee slightly flexed in a neutral valgus and varus position, the hip in neutral, elevating the contralateral leg and bending the hip in 90 degrees of flexion, and controlling this position in a freehand manner). The eyes were opened and closed in order to focus on the neuromuscular feedback system (proprioceptors).
Gait Training: The aim of gait training was to increase intense pronation, weight bearing of the first MTP joint, and weight bearing and push-off of the hallux. Patients had to be able to do a calf raise with complete weight bearing on the big toe and control the correct leg axis while walking on stairs, with a focus on controlling the knee in a neutral position and having enough control of the pelvic region with tension toward abduction and external rotation, which otherwise seems to be the common weak pattern.
Sessions 4, 5, and 6
Based on the individual’s condition, parts of strengthening exercises or sensomotoric training and gait training had to be repeated and increased.
Discussion
-
Hallux valgus is a multicausal pathology.
-
Some consequences are irreversible (surgery) and others modificable like the use of shoes.
-
The treatment needs one global method because of the multiples factors implicated (muscle imbalances, cosmetics reasons, structural, etc).
-
The purpose of this investigation was contributing to the knowledge with this brief review, providing a framework that can be useful for physical therapists and others professionals to optimize their work.
Bibliography
-
Giannini, S., Faldini, C., Nanni, M., Di Martino, A., Luciani, D. & Vannini, F. (2013). A minimally invasive technique for surgical treatment of hallux valgus: simple, effective, rapid, inexpensive (SERI). International Orthopaedics, 37 (9), 1805-13.
Glasoe, W.M., Nuckley, D.J. & Ludewig, P.M. (2010). Hallux valgus and the first metatarsal arch segment: a theoretical biomechanical perspective. Physical Therapy, 90 (1), 110-20.
Kim, M.H., Kwon, O.Y., Kim, S.H. & Jung, D.Y. (2013). Comparison of muscle activities of abductor hallucis and adductor hallucis between the short foot and toe-spread-out exercises in subjects with mild hallux valgus. Journal of Back and Musculoskeletal Rehabilitation, 26 (2), 163-8.
Schuh, R., Hofstaetter, S.G., Adams, S.B. Jr, Pichler, F., Kristen, K.H. & Trnka, H.J. (2009). Rehabilitation after hallux valgus surgery: importance of physical therapy to restore weight bearing of the first ray during the stance phase. Physical Therapy, 89 (9), 934-45.
Another articles in English

|
|
|---|---|
|
EFDeportes.com, Revista
Digital · Año 20 · N° 210 | Buenos Aires,
Noviembre de 2015 |
|